Viruses aren’t living organisms but strands of DNA or RNA that make a home in other living organisms. By doing so, the viruses can survive.
The life-cycle of a virus includes gaining entry into a living organism, replicating, and making itself a home.
Understanding the life-cycle and how the immune system interacts with HPV can better understand why some strains develop into complications like cancer.
What Makes The HPV Life-Cycle Unique?
HPV includes a family of more than 150 types that have slight variations. HPV has adapted over time to target different tissue regions and cause different diseases.
Most HPV infections occur around the mouth or genitals. Some infections cause visible growths like warts and others are asymptomatic.
In addition to the type of HPV strain, symptoms also depend on the individuals’ immune system. The immune system influences how quickly the virus is identified and eliminated from the body. Most HPV infections will complete their life-cycle without causing disease or symptoms at all.
Infection Stage
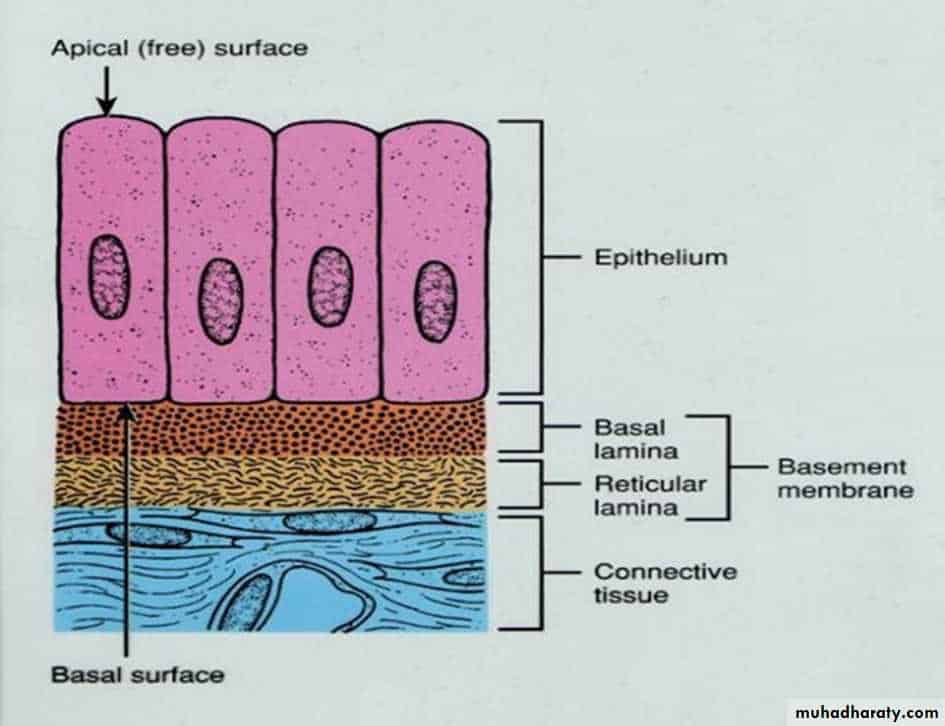
Infection occurs when the HPV gains entry into skin tissue, called epithelial cells. Epithelial cells line the surface of the body and can be classified into three shapes: squamous, columnar, and cuboidal.
When it comes to testing for HPV and cell abnormality, squamous cells are the ones that typically develop abnormalities.
Squamous cells are found in body tissue which forms the very surface of the skin. During a Pap smear, a swab is taken from this layer to examine for abnormalities.
The cells meet the rest of the body through a layer called the basement membrane. This basement layer is where the HPV virus attaches and enters the cell. Once the virus has accessed the cell it can then use the cell to replicate.
Replication:
Depending on the strain of HPV and the body the virus makes a home in, the life-cycle will have different outcomes.
The virus may remain relatively silent. In this case, the virus doesn’t move beyond the basement membrane to cause disease.
The virus may also begin to replicate, releasing its viral particles deeper into the host. When the virus replicates deeper into the skin tissue it is called a productive infection.
Productive Infections
Infections can be classified into grades CIN 1 (deregulated) to 3 (high-grade neoplasia). Persistent high-grade infections at CIN2 or CIN3 can further lead the virus to integrate into the individuals’ genes. This puts the individual at greater risk of developing cancer.
Some areas within the cervix lining are more susceptible to infection. HPV that gain access to the transformational zone in the cervix have been linked to higher rates of cancer progression.
Two viral proteins, E6 and E7, have also been found on high-risk strains of HPV. These proteins are thought to be responsible for stimulating cell cycle entry into the upper epithelial layers and linked to cancerous changes.
Latency
In most cases, HPV will not reach a cancerous state. The majority (80-90%) of HPV infections will clear on their own. Even high-risk strains will likely be cleared by a local immune response.
The virus gets inactivated through interaction with our immune system.
In a healthy immune system, active infections will stimulate immune cells called CD4+ T cells. The presence of CD4+ T cells activates more immune molecules to overtake the virus.
A compromised or weak immune system appears to increase HPV infections.
In viral latency, viral particles continue to exist within the basement membrane in an inactive state. However, the virus can get reactivated following a change in immune status.
What Makes Certain HPV Subtypes More Carcinogenic?
In order for cancer to develop, the virus has to go undetected by the immune system over a prolonged period.
Certain subtypes of HPV, like HPV-16 and 18 are more powerful carcinogens. What makes the virus carcinogenic is its ability to invade the cell layer for longer periods of time allowing changes in the gene expression of the underlying tissue.
It is thought that the presence of E6 and E7 proteins on high-risk strains allows for cervical abnormalities to occur.
How Can You Assist Your Immune System?
It is clear from the research that a healthy immune system is key to preventing HPV infections from reaching a cancerous state.
Diet and lifestyle create the foundation for a healthy immune system. Some important factors in supporting your overall health include:
Optimizing nutrition and supplementation: Consuming fruit and vegetable-rich diet, limiting sugar and refined carbohydrate intake has a positive effect on the immune system.
Managing psychological stress: Prolonged stress can imbalance the ability of the body to fight incoming infections. Engaging in daily stress management practices like meditation, exercise, and socializing can have a positive effect in improving the body’s overall resiliency.
Getting good quality sleep: Getting adequate rest, or seven to eight hours of quality sleep per night allows the immune system time to revitalize. Adequate sleep balances hormones and initiates cellular repair. Setting a regular bedtime, limiting caffeine intake in the afternoon, and eating a nutrient-dense diet are all ways to improve your sleep quality.
Engaging in regular exercise and movement: From improved circulation to naturally increasing the immune cells, staying active has a range of benefits in helping support health and prevent disease. We recommend taking daily walks and engaging in bi-weekly strength training and aerobic activity.